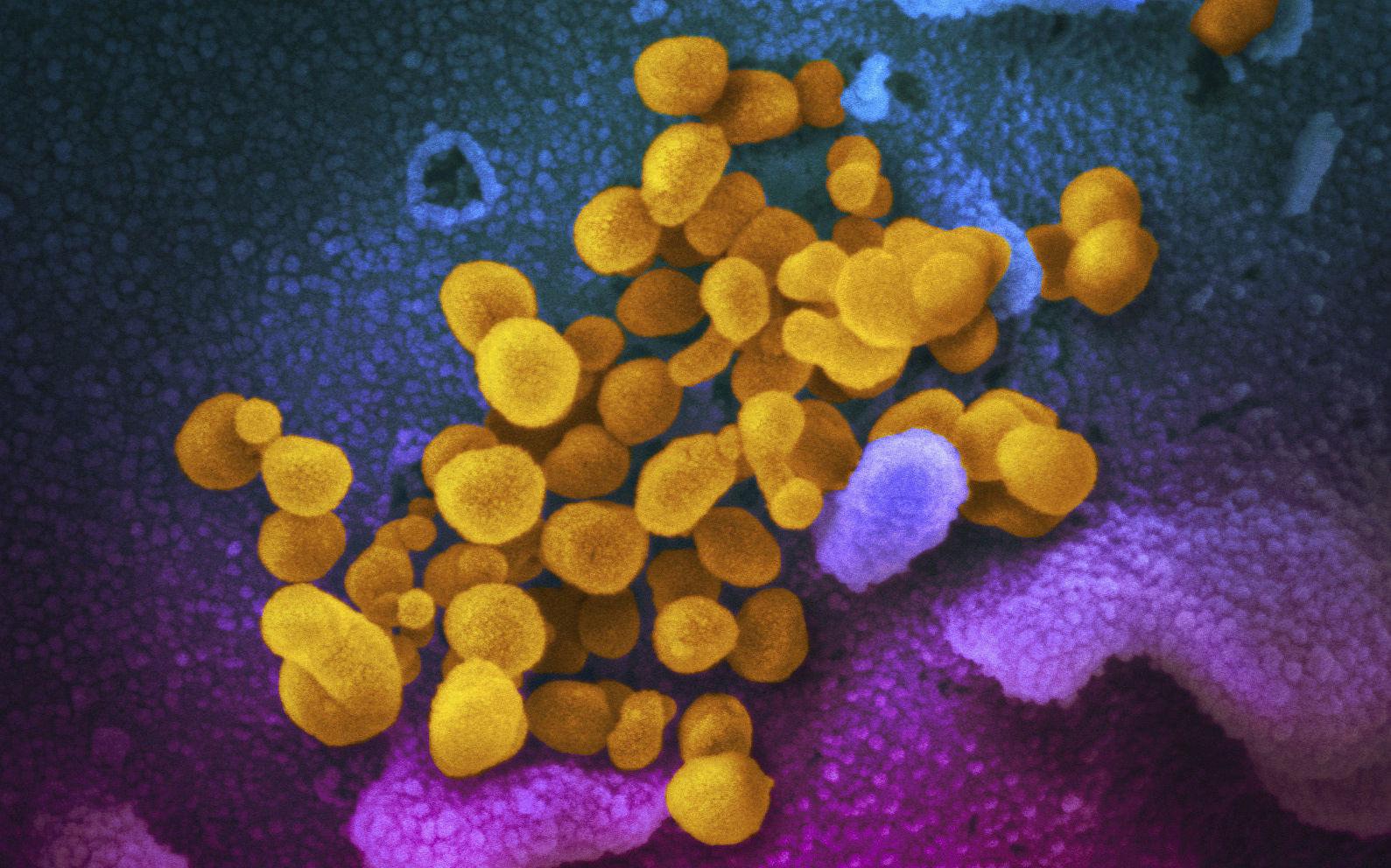
The new and potentially dangerous finding of covid-19 has been discovered in a New study. Corona infection can eventually cause an inflammatory response in the brain, a serious effect that has not been discovered until now.
Researchers at the University of Queensland in Australia investigated the long-term effect of the virus on immune cells in the brain. These are the main cells in the development of brain diseases such as Parkinson’s and Alzheimer’s.
The main finding is that covid-19 activates the same reaction in the brain as Parkinson’s disease. This means that people who have contracted the virus have a higher potential risk of developing neurodegenerative diseases.
– We found that the cells became angry
Examples of neurodegenerative diseases include Parkinson’s disease, Alzheimer’s disease, and Huntington’s disease. These are pathological conditions that cannot be cured and involve a gradual deterioration of the general condition. Certain groups of neurons gradually die, die, or change function during the course of the disease.
We found that the cells became angry and activate the same thing that Parkinson’s and Alzheimer’s proteins can do. The effect of Covid infection is exacerbated if there are already proteins in the brain associated with Parkinson’s disease. It’s like pouring gasoline on a fire that has already started in the brain. That’s what makes it so dangerous, says Professor Trent Woodruff of the University of Queensland’s Department of Biomedicine in Australia. News.com.
The disease begins in the brain up to 15 years noticeable symptoms
Woodruff led a team with colleague Professor Eduardo Albornoz Balmaceda and virologists from the School of Chemistry and Molecular Biosciences. The study has now been published in the scientific journal Molecular Psychiatry.
Alzheimer’s disease spreads at different speeds to the entire brain and eventually leads to death. The course of the disease is characterized by a gradual deterioration. The disease begins in the brain until the age of 15, before symptoms of the disease are detected, according to what he reported Great Norwegian Dictionary.
Changes occur around neurons in and within the cerebral cortex, but also in the deeper parts of the brain. Cells are damaged and die. This causes the brain to gradually become smaller.
– He’s a silent killer
According to Professor Albornoz Balmaceda, it may take many years before symptoms appear. Thus, the long-term consequences after a confirmed infection with the Covid-19 virus cannot appear until several years later.
It’s a silent killer because you haven’t seen any external symptoms for many years, says Palmaida.
Parkinson’s disease results from the destruction of brain cells that help control movement. Symptoms can creep in, and it can take time to get the right diagnosis, accordingly HNI- No. The lack of dopamine leads to complaints such as slow and sluggish movement, increased degree of stiffness of the arms and legs, tremors that particularly affect the hands.
A drug that can stop encephalitis
The new study may explain why some people with COVID-19 are more likely to develop neurological symptoms similar to Parkinson’s disease or develop dementia.
But the study also carries good news for those affected. Clinical studies are now underway in Parkinson’s patients with a drug that can stop the inflammation in the brain caused by COVID-19 infection.

“Explorer. Unapologetic entrepreneur. Alcohol fanatic. Certified writer. Wannabe tv evangelist. Twitter fanatic. Student. Web scholar. Travel buff.”