This problem is called aberration, or imaging error. Now solved, next-generation cardiac ultrasound technology is on its way to the world with NTNU and GE Vingmed Ultrasound technology.
The innovation is named Adapt. It is basically an algorithm that uses raw data from ultrasound to estimate and compensate for the effect of body tissues in each individual patient.
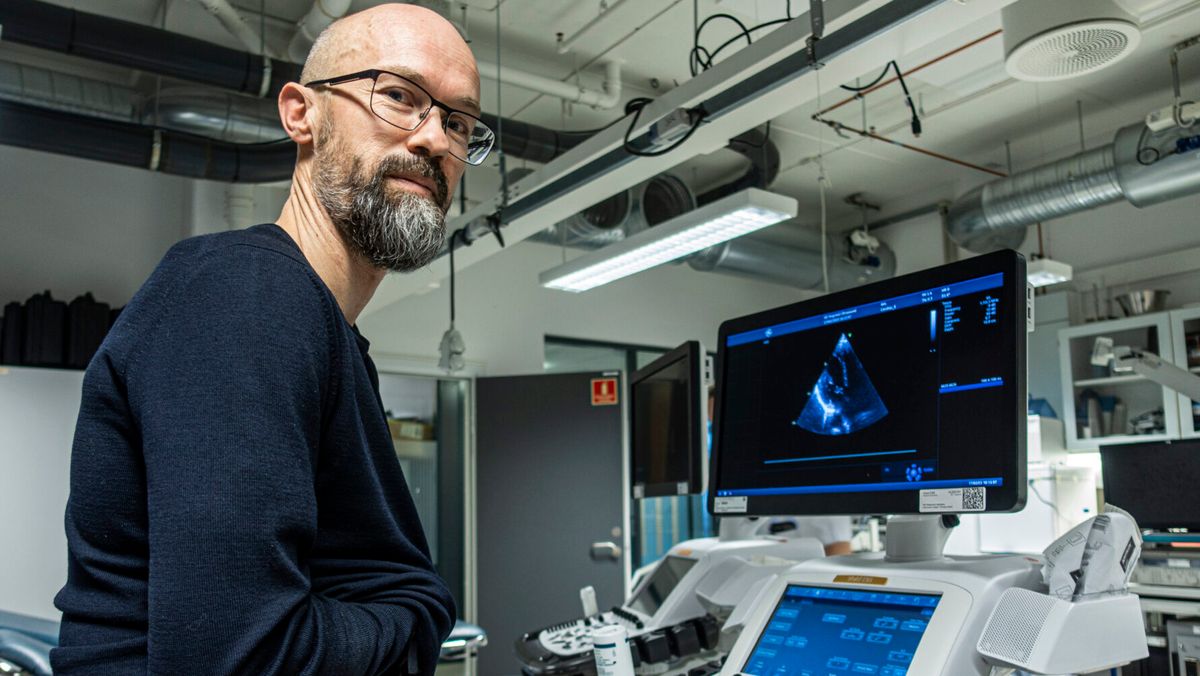
– It provides sharper, clearer images of the heart than we’ve seen before, says Svein-Erik Måsøy, a researcher, medical ultrasound expert and director of SFI CIUS (Center for Innovative Ultrasound Solutions) at NTNU.
18 million deaths annually
According to the World Health Organization (WHO) About 18 million people die cardiovascular disease every year. The incidence rate has doubled in 30 years and it tops the list of the world’s greatest health challenges. More than 100 million heart examinations using ultrasound are performed each year.
Disorders often come with age. Here at home, the elderly wave has just begun.
– The numbers say something about the scale of the challenges we’re working on, and about the market our technology is now a part of, says Måsøy.
– We are the first in the world to come up with this solution. In our niche, this is definitely a breakthrough. He says time will tell what that means in the heart clinic.
SFI CIUS is one of twelve Centers for Research-Driven Innovation (SFI) led by NTNU. Adapt is marketed by Horten GE Vingmed Ultrasound.
GE Wingmed ultrasound machine and adaptation
- GE Vingmed Ultrasound in Horton is part of GE HealthCare.
- The company is the world leader in cardiac ultrasound equipment.
- The company has approximately 40 percent market share. 8 billion US dollars (about NOK 85 billion).
- Every day, 300,000 hearts are scanned with an ultrasound machine from GE Vingmed.
- The SFI CIUS team validated the Adapt technology against a database of raw data from more than 30,000 echocardiographic images collected at the clinic.
- Systems that can use Adapt are used only in the largest and most advanced hospitals.
- NTNU Technology Transfer was responsible for licensing Adapt.
The main challenge: the different bodies
Ultrasound is sound converted into images. The biggest challenge of diagnosing a heart with ultrasound is that people have different bodies. We have different muscles and different connective tissues, and both the amount and distribution of subcutaneous fat is different. The distance between our ribs varies with height, age and gender.
All this results in different speeds of sound waves, and it is the speed that determines the quality of ultrasound images.

Svein-Erik Måsøy compares sending ultrasound through the body’s tissues to imaging with a layer of Vaseline on the lens. Contrasts disappear, and the image becomes cloudy. So the problem is called deflection. What Adapt does is estimate and compensate for the effect of Vaseline and give us a clearer, clearer picture.
Assist in safer diagnosis
Real-time image quality is particularly important for myocardial infarction. Very small changes in the way the heart muscle moves can tell doctors something about the extent and damage of the infarction. Chief Physician Bjornar Green, who works in the Echo Department of the Cardiology Clinic at St Olav’s Hospital, confirms that Adapt generally contributes to the improvement of ultrasound images.
– Especially in patients where it’s hard to get good enough images, we see a difference. It is precisely in those cases that we need such an improved method.
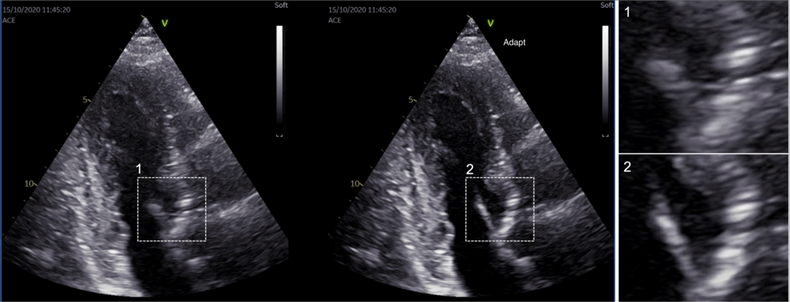
For example, the heart valves become more visible. This also applies to the distinction between myocardium and heart chamber. This makes it easier to see the structures of the heart, which can provide more accurate measurements and safer diagnoses. Green says this is important for giving each patient the best possible treatment.
The cardiologist is also a researcher at SFI CIUS and chair of the Norwegian Society of Cardiology Working Group on Echocardiography.
Many people can get really bad photos
When the ultrasound probe is placed on the patient’s chest, sound waves are directed toward the heart. On its way to the fabric, the waves are reflected as echoes. The probe contains thousands of sensors that act as speakers and microphones. This instrument helps to determine the exact source of the sound.
All the data is put into a huge computational process and the sound is converted into an image. When the texture or material through which the sound passes is the same everywhere, this happens smoothly. But the variety of bodies means that the image quality may be very poor for 10-15% of all those examined. This could mean that 10-15 million patients do not receive the best possible treatment – every year.
Huge amounts of data
In the early 2000s, Svein-Erik Måsøy worked on his Ph.D. on new methods for improving calculations of deviations. The methods worked, at least in theory.
– General Electric had a demonstrator of the technology in 2000. The computer used was the size of the ultrasound machine itself, and thousands of cables ran between them, says Måsøy.
They were able to correct one to two images per second. Today, it is possible to correct up to 150 images per second.
“Back then everything became so far-fetched, as well as too expensive, and the project fizzled out,” says Måsøy, who defended his Ph.D. in 2004.
And now it’s time to introduce those who have finally become ultrasound researchers’ new friends: gamers and the computer game industry.
The gaming industry was crucial
In recent years, developments in the gaming industry have evolved dramatically. Microprocessors or Graphics Processing Units (GPUs), which were originally designed to display images on a screen, have been greatly improved.
It works incredibly fast, has huge computing power and a comparable amount of memory. GPUs are coming in increasingly better versions and are becoming off-the-shelf products that are also used by other industries. The gaming industry now has a turnover of US$150 billion annually.
– Image processing is now so fast that all seasons of your favorite Netflix series rush through the ultrasound machine in one to two seconds, says Måsøy.
Perfect effort for better pictures
Within the framework of SFI CIUS, a core team of ten researchers from NTNU, the University of Oslo, GE HealthCare and St Olav’s Hospital again tackled the problem of imaging errors. Hardware from the gaming industry has taken care of the intensive processing of raw data, while researchers can focus on how to improve ultrasound images of the heart.
Advances in 3D medical imaging have also made great strides.
All this led to adaptation. Four cardiologists at St Olaf’s Hospital tested the new technology in a pilot study. In 97 percent of the tests, they preferred the adaptation to what was, at the time, the best equipment available. Bjornar Green participated in the study. He also made several ultrasound recordings and image analyzes.
– In choosing between registering with Adapt vs. without, I will always prefer Adapt. He says that the reason for this is that the quality of ultrasound images of the heart is improving, and this is critical for the analyzes and diagnostics that I will do.
Here Svein-Erik Måsøy explains how SFI CIUS corrected image errors:
40 years of cooperation
GE began developing Adapt in 1989. NTNU has been working on the problem since the early 1990s. Professors Bjorn Angelsen and Leif Hatley were among the pioneers in developing the Doppler technique, among others.
“The close collaboration between GE Vingmed and NTNU in recent decades has been crucial to ensuring that GE Healthcare remains the best in the world for quality ultrasound,” says Bastien Dénarié, development engineer at GE HealtCare.
The collaboration contributes to the development of unique technologies such as Adapt, but also to the creation of a network of engineers in Norway specializing in imaging ultrasound and signal processing.
The article was first published on Gemini

“Web specialist. Lifelong zombie maven. Coffee ninja. Hipster-friendly analyst.”